A single-institution, review partner study revealed the rate of opportunistic infections among patients with hematological malignancies who got ibrutinib and distinguished potential patient hazard factors. The study discoveries were published online May 13, 2019, in Leukemia.
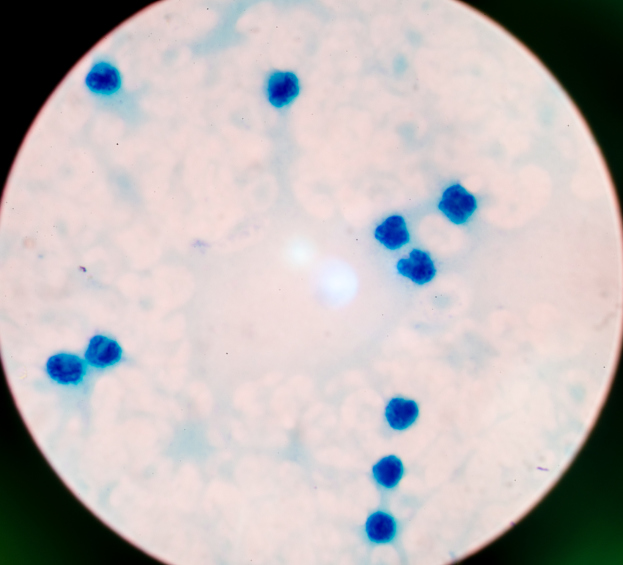
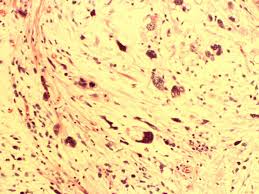
The records of 566 patients with hematologic malignancies who got ibrutinib between June 2010 and March 2016 were reflectively explored for occasions of opportunistic infection, which included pneumocystis jirovecii pneumonia, intrusive and dispersed fungal infections, dynamic multifocal leukoencephalopathy, toxoplasmosis, viral disseminated infections, and atypical bacterial infections.
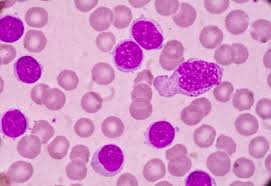
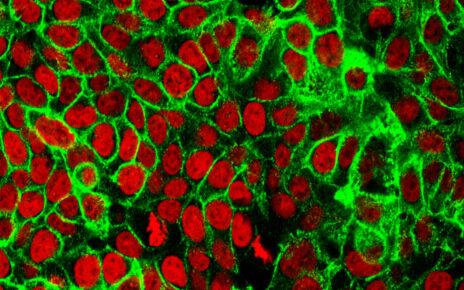
Most patients (80.9%) were clinical preliminary members, most had chronic lymphocytic leukemia (73.7%), and 30.9% got ibrutinib in combination with another agent, with an anti-CD20 monoclonal antibody being the most common agent (81.7%).
Generally speaking, the companion had 1225 patient-years of ibrutinib presentation and the middle introduction for an individual patient was 1.98 years (range, 0.008 – 6.40 years).
At a middle follow-up of 2.69 years (range, 0.03-6.40 years), 23 instances of opportunistic infections happened, which yielded an incidence rate of 1.9 per 100 man years (95% CI, 1.2-2.8). A large portion of the opportunistic infection cases were invasive fungal infections (17 patients, 73.9%), with invasive aspergillosis being the most common type (12 patients, 52.1%). From the time of opportunistic infection diagnosis, the median survival was 1.39 years (95% CI, 0.38-not came to).
As indicated by a multivariate analysis, receipt of at least 3 earlier lines of treatment (hazard ratio [HR], 2.87; 95% CI, 1.12-7.35; P =.028), diabetes (HR, 3.63; 95% CI, 1.50-8.77; P =.004), and liver disease (HR, 7.53; 95% CI, 2.14-26.49; P =.002) were each autonomously connected with building up an opportunistic infection amid ibrutinib treatment.
“In conclusion, we found that invasive fungal infections occur at a low frequency during ibrutinib therapy, with aspergillus being the most common infectious organism,” the study authors wrote. “Further work is needed to confirm risk factors and determine the optimal monitoring and prophylaxis for these patients.”