An epic nanovaccine has shown adequacy in anticipating the improvement of melanoma in mouse models, just as in treating primary tumors and metastases that outcome from melanoma.1 This leap forward could make ready for a really successful melanoma immunization approach that may even demonstrate valuable in the most progressive phases of the illness.
“In our study, we have shown that it is possible to produce an effective nanovaccine against melanoma and to sensitize the immune system to immunotherapies,” says Prof. Ronit Satchi-Fainaro, seat of the department of physiology and pharmacology and leader of the Laboratory for Cancer Research and Nanomedicine at Tel Aviv University Sackler Faculty of Medicine, Tel Aviv, Israel, who co-drove the research.
In a cooperative exertion between Prof. Satchi-Fainaro’s group and individual associates from the Research Institute for Medicines (iMed.ULisboa), personnel of drug store, Universidade de Lisboa, Lisbon, scientists built up a sharp nanovaccine for melanoma that accomplished great therapeutic results in mice.
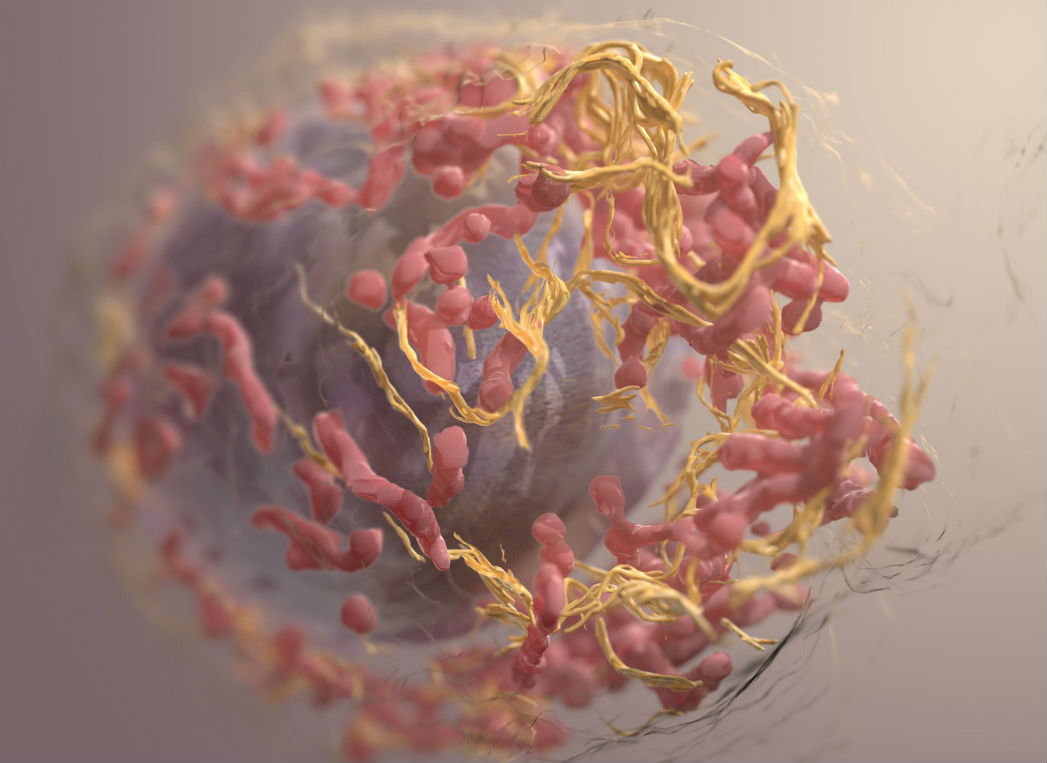
Subsequent to outfitting little particles of roughly 170 nanometers in size, made of biodegradable polymer, they stuffed every molecule full with two peptides, or short chains of amino acids, that are likewise communicated in melanoma cells. The nanoparticles or “nanovaccine” were then infused in a mouse model bearing melanoma.
“The nanoparticles acted just like known vaccines for viral-borne diseases. They stimulated the immune system of the mice, and the immune cells learned to identify and attack cells containing the two peptides, that is, the melanoma cells. This meant that, from now on, the immune system of the immunized mice will attack melanoma cells if and when they appear in the body,” Prof. Satchi-Fainaro says.
The nanovaccine was tried under different conditions and was seen as successful in anticipating the advancement of melanoma, deferred the advancement of the disease, and seemed to work in forestalling or slowing brain metastases. Scientists infused healthy mice with the nanovaccine, and afterward melanoma cells, whereupon the mice stayed healthy.
A blend of the vaccine and immunotherapy medicines was additionally used to treat the primary tumor. Results demonstrated that the synergistic impact of the blend treatment fundamentally postponed the movement of the disease and extraordinarily expanded the lives of every treated mouse. The analysts likewise approved their methodology on tissues taken from patients with melanoma brain metastases, proposing that the nanovaccine can be utilized to treat mind metastases also.
Advances in immune treatment for melanoma have improved treatment results dependent on antitumor immune reactions inspired by the patient’s very own immune system. Be that as it may, a low reaction rate, obtained obstruction and extreme symptoms have constrained the clinical results of immune checkpoint treatment. With the clinical victories accomplished with CTLA-4 (cytotoxic T-lymphocyte-related protein-4) and PD-1 (customized cell demise protein 1) bar in upgrading explicit T-cell-intervened antitumor immunity, endeavors have now been made to invigorate the signaling pathways of the immune system.
“The war against cancer in general, and melanoma in particular, has advanced over the years through a variety of treatment modalities, such as surgery, chemotherapy, radiation therapy and immunotherapy; but the vaccine approach, which has proven so effective against various viral diseases, has not materialized yet against cancer,” Prof Satchi-Fairnaro says.
“Our research opens the door to a completely new approach – the vaccine approach – for effective treatment of melanoma, even in the most advanced stages of the disease. We believe that our platform may also be suitable for other types of cancer and that our work is a solid foundation for the development of other cancer nanovaccines,” Prof. Satchi-Fainaro finishes up.